Root Canal Therapy
Save your natural tooth and relieve pain
Root Canal Therapy
Save your natural tooth and relieve pain

Professional care for infected or damaged teeth
Don’t lose it! A tooth infection or severe decay doesn’t have to end in extraction. Root canal treatment gently removes the infection, preserves your natural tooth, and helps you bite and smile with confidence again.
Using advanced techniques and gentle care, our experienced dentists can help bring your tooth back from the brink. They carefully remove the infected pulp, disinfect and seal the canals, and restore the tooth’s integrity with a durable crown or filling. This comprehensive approach relieves pain, eliminates infection, and preserves the full function and aesthetics of your natural tooth.
What is root canal therapy?
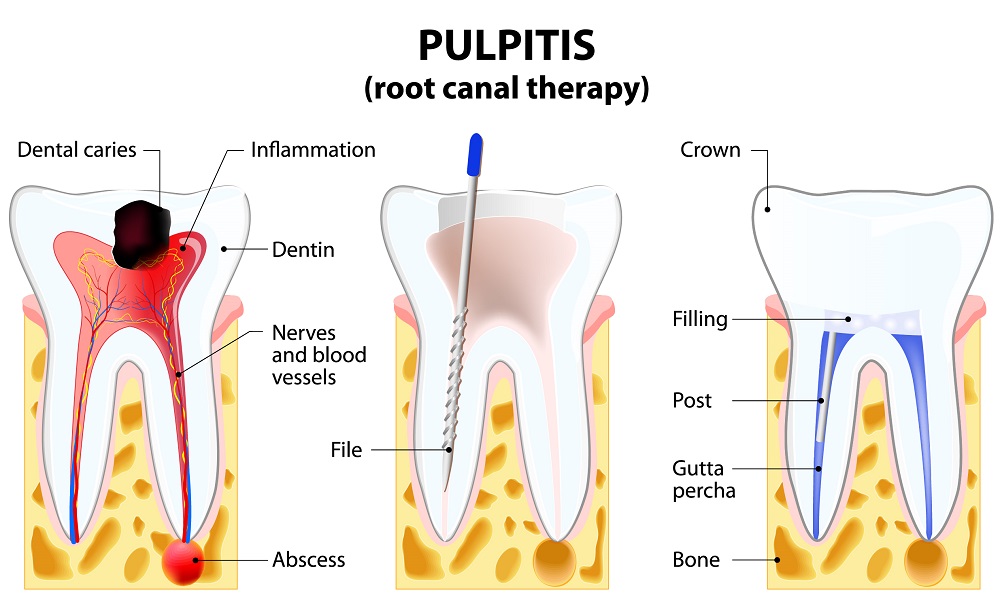
Root canal therapy (RCT) is a dental procedure designed to save a tooth that is infected, inflamed, or severely damaged. Rather than removing the tooth, the treatment involves removing the diseased pulp, which is the soft tissue inside the tooth that contains nerves and blood vessels, and thoroughly cleaning and disinfecting the root canals to eliminate infection.
Once the canals are sealed to prevent reinfection, the tooth is restored with a dental filling or crown, which restores its strength, function, and appearance, allowing it to continue performing like a healthy natural tooth.
How tooth pulp affects oral health
Each tooth contains a soft inner core called the pulp, which is made up of nerves, blood vessels, and connective tissue that support the tooth’s development and vitality. The pulp extends through narrow canals in the tooth roots and connects to tissues in the jawbone.
If bacteria enter the pulp — often through deep decay, cracks, fractures, or advanced gum disease — it can cause inflammation or infection. Untreated infections may spread beyond the root, potentially leading to abscesses, severe pain, and swelling in the surrounding gum, jaw, or face.
If the pulp is only inflamed, it may sometimes be preserved, but a fully infected pulp usually needs to be removed. The good news is that once the infection is treated or the damaged pulp is removed and a cap or crown is placed, the tooth can continue to survive and function normally, supported and nourished by the surrounding gum and bone tissues.
Common causes of pulp infection
A root canal may be required if your tooth has been affected by:
- Deep tooth decay that reaches the nerve chamber.
- Cracked or fractured teeth from trauma or teeth grinding (bruxism).
- Repeated dental procedures on the same tooth.
- Advanced gum disease spreading to the tooth’s root.
- Dental injury that exposes or damages the pulp.
- Common signs you may need a root canal include:
- Persistent or throbbing tooth pain.
- Sensitivity to hot, cold, or sweet foods and drinks.
- Pain when chewing or touching the tooth.
- Gum swelling or a pimple-like bump near the affected tooth.
- Tooth discolouration or darkening.

Why not wait for natural healing?
When the pulp becomes infected, it cannot heal on its own. Without treatment, the infection can spread and may eventually require tooth extraction. A root canal allows your dentist to:
- Remove the source of infection and pain.
- Preserve your natural tooth.
- Prevent further damage to the surrounding bone and gums.
- Restore your ability to chew comfortably.
What to expect during root canal treatment
Root canal therapy is usually completed over two to three visits, depending on the level of infection and the type of restoration needed.
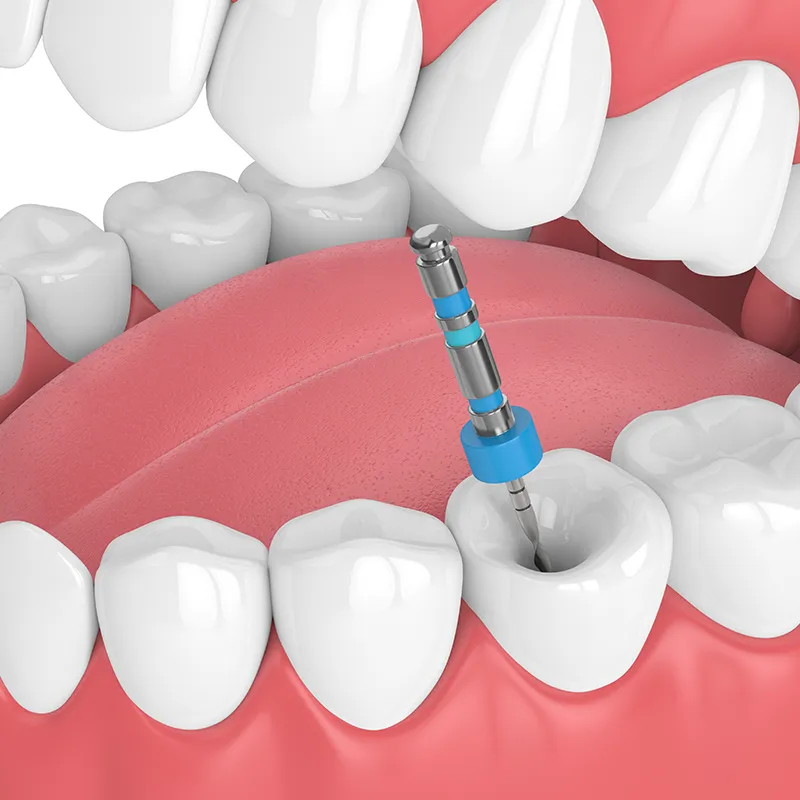
1. Removing the infected pulp
After administering local anaesthesia, your dentist will create a small opening in the tooth to access the root canals. The infected or dead pulp — which contains nerves and blood vessels — is carefully removed. This step relieves pressure inside the tooth and eliminates the source of pain. Once the pulp is removed, the tooth no longer has a blood supply, which is why it can become more brittle over time.
2. Cleaning and shaping the canals
Next, the root canals are thoroughly cleaned and disinfected to eliminate bacteria and infected tissue. The canals are then shaped precisely to prepare them for filling. This stage is crucial to ensure that the entire canal system is free of infection and can be completely sealed.
3. Filling and sealing
Once the canals are clean and dry, they are filled with a biocompatible, rubber-like material called gutta-percha. This material seals the canals and prevents bacteria from re-entering the tooth. A temporary filling is then placed to protect the tooth until the final restoration.
4. Final restoration
To restore full function and strength, the treated tooth is covered with a permanent filling or dental crown. In most cases, a crown is recommended, as it provides long-term protection against fractures and restores the tooth’s appearance and chewing ability.
Mild tenderness or sensitivity may occur for a few days after treatment — this is normal and can usually be managed with over-the-counter pain relief. Good oral hygiene and regular dental check-ups help keep the treated tooth healthy for many years.

Reasons to consider root canal treatment

- Save your natural tooth from extraction
- Relieve pain and discomfort caused by infection
- Restore normal chewing function and bite strength
- Prevent the spread of infection to surrounding teeth or tissues
- Maintain natural tooth alignment and jawbone integrity
- Support long-term oral health and overall wellbeing
- Preserve the natural appearance of your smile
Understanding the Risks and Rewards
Root canal treatment is a common and effective procedure, and while its benefits generally outweigh the risks, a few possible side effects are worth noting.

- Weakened tooth structure can occur because the treated tooth no longer receives nutrients through its pulp. A dental crown is strongly recommended to protect it from fractures and restore normal chewing function.
- Tooth discolouration may develop over time due to the loss of blood supply after treatment. In some cases, internal bleaching can be performed to brighten the tooth from within and restore its natural colour.
- Persistent infection is uncommon but possible if bacteria remain in complex root structures. In such cases, retreatment or a minor surgical procedure (apicoectomy) may be required to fully resolve the infection and save the tooth.
With proper care, most patients enjoy long-term comfort and function from their treated tooth. Regular check-ups are an important part of achieving lasting results and protecting your overall oral health for the long term.
Root canal treatment FAQs
1. How do I know if I need a root canal?
You may need treatment if you experience a persistent toothache, sensitivity to hot or cold, pain when chewing, gum swelling, or a darkened tooth. Your dentist will examine your tooth and take X-rays to confirm if treatment is necessary.
2. Is a root canal painful?
Root canal procedures are performed under local anaesthesia, so discomfort during treatment is minimal. Some mild soreness or tenderness can occur for a few days afterwards, which can usually be managed with over-the-counter pain relief.
3. How long does a root canal take?
Most treatments are completed in 1–3 visits, depending on the complexity and the tooth involved. Each visit typically lasts 30–90 minutes, covering cleaning, shaping, and sealing of the canals.
4. Can a root canal save my tooth?
Yes. Treatment removes the infection while preserving your natural tooth. Once restored with a filling or crown, most treated teeth can last a lifetime with proper oral care.
5. What are the alternatives to a root canal?
Without treatment, an infected tooth may eventually require extraction. Replacement options afterwards include dental implants, bridges, or partial dentures.
6. How should I care for my tooth after treatment?
Maintain good oral hygiene, brush and floss daily, and avoid chewing hard foods on the treated tooth until it is fully restored. Regular dental check-ups help ensure long-term success.
7. Can a root canal fail?
Although success rates are high, infection can sometimes recur due to untreated canals, complex root anatomy, or delayed restoration. If this happens, retreatment or a minor surgical procedure called an apicoectomy may be recommended.
8. Will my tooth change in appearance?
Yes, some teeth may gradually darken after root canal therapy due to the loss of internal blood supply. This is normal and doesn’t affect the tooth’s function. If discolouration occurs, a crown, veneer, or internal bleaching can be used to restore a natural appearance and protect the tooth from potential fractures.
9. How long will the tooth last after treatment?
With proper oral hygiene, regular dental check-ups, and a well-fitted crown or filling, a tooth that has undergone root canal treatment can last for many years. Longevity depends on factors such as the tooth’s condition, the quality of restoration, and ongoing care.
10. How much does a root canal cost?
Costs vary depending on the tooth, complexity, and restoration needed. Your dentist will provide a personalised treatment quote and discuss available payment options during your consultation.
Persistent tooth pain? See the dentist ASAP
If your teeth or gums have persistent pain, sensitivity, or signs of inflammation, don’t wait until it worsens. Early assessment and treatment can save your tooth, prevent infection from spreading, and reduce the chance that you may need more invasive procedures. In short, get discomfort checked early!
Don’t wait in pain. Our team at Healthy Smile Dental is here to help — book your consultation today.
